By Michael Reinhorn MD, MBA, FACS
As a surgeon with over two decades of experience, I’ve witnessed the healthcare landscape undergo significant changes, and 2023 has proven to be particularly challenging, especially for independent specialty surgical practices like ours at Boston Hernia.
At Boston Hernia, we specialize in abdominal core health. We have mastered two approaches to inguinal hernia repair that are better for patients and are not commonly performed. This has virtually eliminated chronic pain – a problem affecting 30,000 Americans who undergo inguinal hernia repair each year. Our practice, co-founded in 2018 by physician assistant Lauren Ott, PA-C, and me, is driven by a mission to create a scalable and replicable model for achieving the highest quality of patient care while simultaneously training other surgeons in our innovative approach.
A startling one in 30 hernia surgery patients in the United States endures permanent injury, and 5 to 15% experience temporary disability lasting up to a year after inguinal hernia repair. My extensive experience reveals that these complications are almost entirely preventable.
Over the past five years, we at Boston Hernia have cared for hundreds of patients annually, meticulously researching and publishing our outcomes in international journals to share our knowledge with the broader surgical community. Despite the challenges of operating independently, we’ve thrived by prioritizing patient well-being and financial transparency. In fact, we actively encourage patients to utilize lower-cost facilities when appropriate, ensuring the best possible care at the most affordable price.
We recruited Dr. Nora Fullington, an outstanding and experienced surgeon, to our practice in 2021. Within four months, Dr. Fullington was expertly trained in open preperitoneal inguinal hernia repair, a less invasive procedure utilizing sedative anesthesia instead of general anesthesia. 2023 has been a resounding success for Boston Hernia, marked by academic achievements and an increased patient volume. By the end of the year, we will have seen over 1500 new patients, operated on more than 850 of them, and repaired over 1000 hernias.
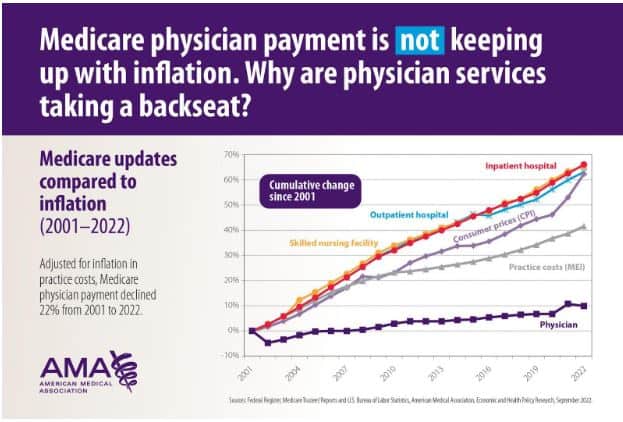
Despite our clinical success, the healthcare system’s structure has forced us to make drastic changes to remain financially viable. Over the past two decades, Medicare and other health insurers have shifted funding towards facilities, specifically hospitals. Simultaneously, provider reimbursement has remained stagnant (or, in some instances, has decreased) despite significant inflation, rising consumer goods costs, and labor expenses. The combination of escalating practice expenses and stagnant reimbursement has driven many physicians to abandon independent practices in favor of employment by larger hospital systems or private equity groups, seeking the subsidies provided by increased hospital reimbursements. This can be seen in the visual below.
The corporatization of healthcare, the moral dilemmas faced by employed physicians, the alarming burnout rate within the industry, and recent reports of large hospital systems turning away patients due to provider shortages have been well-documented in the news. Boston Hernia, as an independent practice, has consistently prioritized patients and providers. Until 2023, our practice was immune to burnout, as we were confident in and found fulfillment in our patient-centric approach and fair compensation of all employees, providers, and front office staff.
However, 2023 brought about two seismic events that forced drastic changes at Boston Hernia. First, CMS reduced physician reimbursement for smaller abdominal wall hernias, regardless of complexity, to a uniformly low rate of $362. This change disproportionately impacted physicians compared to hospitals, resulting in a 10% revenue decline across the board for our practice. Additionally, large hospital systems, facing increased financial pressures, began restricting patient referrals to independent, high-quality practices, aiming to retain revenue within their networks, regardless of care quality.
Initially, we attempted to negotiate with national payers who had adopted Medicare rates, which were unsustainable for our practice. Our efforts to increase our reimbursement rates were met with ridicule from physician administrators within these large insurance companies. As a result, we opted out of contracting with these companies, and surprisingly, our patients remained loyal and willing to pay a reasonable out-of-pocket expense to ensure we were appropriately compensated. For each hernia repair, we charge $2,250, covering the surgeon and an expert assistant for the procedure itself. Most patients still utilize insurance to cover hospital, surgical center, and anesthesiology costs.
After careful consideration, I made the difficult decision to opt out of Medicare. While morally challenging, it was the only viable option to resuscitate Boston Hernia and continue to provide excellent, timely, and inexpensive care to hernia patients in our community. The immediate change in the payer mix transformed our practice from financial instability to a sustainable practice, poised for continued growth.
I fervently hope that Boston Hernia’s independence will endure, enabling us to contribute to resolving the healthcare system’s critical flaws. I envision a future where Boston Hernia continues to provide the highest quality care, trains more surgeons in advanced hernia repair techniques, and expands our services to include patients with limited financial means. While this transformation may take decades, I am optimistic that we can achieve our goals and accomplish our mission, all while demonstrating that patients’ needs can be placed first while maintaining a financially viable business model where providers are happy to work.
