Wellesley Massachusetts, November 2021
By Bailey Pate & Michael Reinhorn
Last month Dr. Rosen, a colleague of Dr. Reinhorn, flew up to Boston in order to observe Dr. Reinhorn and his new associate, Dr. Nora Fullington, perform both the Shouldice no mesh inguinal hernia repair and the open preperitoneal inguinal hernia repair.

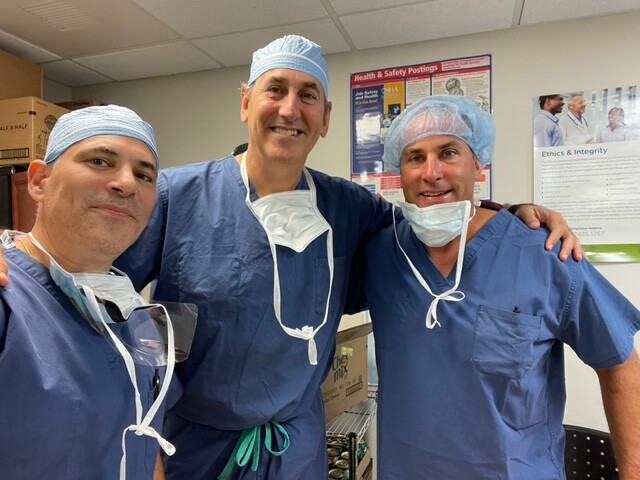
Drs Reinhorn, Rosen and Fullington (Left to right)
First, some background about the surgeons. Dr. Michael Rosen is a past president of Americas Hernia Society and currently he is a co-founder and president of the Abdominal Core Health Quality Collaborative (ACHQC). This collaborative is a non-profit organization that acts as a national hernia registry for the United States. It was modeled after European hernia registries, and allows surgeons to voluntarily report data on their patients having surgery in order to aggregate data and identify opportunities for improved care. The United States FDA has partnered with the ACHQC in order to monitor the quality of mesh implants. Several years ago, the ACHQC was first to detect a problem with a particular product which led to a recall. This partnership with the ACHQC and the FDA puts patients’ safety first!
In addition to his responsibilities with the ACHQC, Dr. Rosen is a very busy abdominal wall surgeon, leading a group of 6 hernia surgeons as well as a fellowship program at the Cleveland Clinic. He is also an accomplished academic who has given multiple national and international podium presentations, and has published numerous papers and written multiple book chapters.
Dr. Michael Reinhorn is an inguinal hernia specialist and has been in private practice for 20 years. Over that time, he has identified opportunities for improvement in the care of ambulatory hernia patients which led him to establish Boston Hernia several years ago. The aim of the practice is to advance the science of ambulatory hernia surgery and improve the patient experience. Dr. Reinhorn has led the opioid reduction task force for the ACHQC and has co-authored several papers related to this subject matter. The efforts of the task force have allowed for significant reduction in the number of opioid medications prescribed after hernia surgery and contributed to the national effort to reduce opioid addiction.
Dr. Reinhorn was able to pinpoint the deficit in hernia education in the United States which leads to unacceptably high rates of long-term disability after ambulatory inguinal hernia surgery. Three percent of patients experience lifelong disability and five to fifteen percent of patients experience disability for up to one year after these procedures. In 2016, while studying for a Masters in Business Administration, Dr. Reinhorn visited The Shouldice Hospital to learn both their surgical techniques and business practices. Dr. Reinhorn incorporated the Shouldice technique into his practice in 2016, and even had one of his MBA colleagues, Dr. Samer Sbayi, who at the time was a Shouldice employed surgeon, observe him in the OR. The purpose of this experience was to provide Dr. Reinhorn with invaluable feedback to improve his technique. Dr. Reinhorn serves on the board of the ACHQC and is a member of the American Board of Surgery committee for oral exams pertaining to hernias. Dr. Reinhorn also serves various leadership roles at Newton-Wellesley Hospital, which is a part of the Mass General Brigham system.
Dr. Nora Fullington is an accomplished surgeon with over 5 years of experience in general surgery and since early 2021 has worked as a specialized hernia surgeon at Boston Hernia. Dr. Fullington joined the Boston Hernia team with years of extensive surgery experience in both open and laparoscopic hernia repair. Initially after joining Boston Hernia, Dr. Fullington studied intensively under Dr. Reinhorn, and quickly became an expert both in the Shouldice and open preperitoneal inguinal hernia repairs and has transitioned to teaching the repair to other surgeons. She has particular interest in global surgery efforts and has led mission trips to Haiti where there is significant need for surgical care of patients with hernia. She has also joined the ACHQC and participates in the efforts to constantly improve the quality of care in the treatment of hernia and reduction of excess opioid prescribing.
In September of 2021, Dr. Rosen visited the Boston Outpatient Surgical Suites in Waltham, Massachusetts in order to observe Dr. Reinhorn and Dr. Fullington independently perform these repairs. The goal of Dr. Rosen’s visit was to observe 3 Shouldice operations, the first of which was performed by Dr. Reinhorn, followed by two performed by Dr. Fullington. Dr. Rosen also had the added benefit of being able to observe Dr. Fullington perform an open preperitoneal repair. In order to facilitate Dr. Rosen’s learning, Dr. Reinhorn narrated the procedure in detail for all four operations in order for Dr. Rosen to have the best experience in learning. When Dr. Reinhorn visited the Shouldice hospital, he was struck by the fact that each surgeon performed the operation in the exact same way. Dr. Rosen observed Dr. Fullington performing hernia repair in the exact same way, much like the Shouldice tradition.

Dr. Michael Rosen learning from Dr. Fullington and Lauren Ott, PA-C
Earlier this month, Dr. Rosen was able to complete his first Shouldice operation at the Cleveland Clinic. Despite Dr. Rosen’s training at Massachusetts General Hospital, his extensive practice at the University Hospital at Cleveland and Cleveland Clinic Foundation, he found that the dissection performed by Dr. Fullington was nothing like he had ever seen before. He described the dissection as being more extensive, more meticulous, and with better defined anatomy than anything he had ever seen in the groin in the past. Given the fact that he had the opportunity to observe Dr. Fullington, he also felt that she is an excellent technical surgeon and clearly has mastered the language of hernia anatomy and dissection. During this experience, Dr. Rosen saw all three nerves typically seen in the anterior dissection each and every time during surgery. Dr. Rosen commented that seeing the ilioinguinal, genital branch of genitofemoral, and iliohypogastric nerves have been challenging in the past, but not any longer.
Dr. Reinhorn’s reflections:
This visit by Dr. Rosen had a significant impact on me. It was the second time I had the opportunity to teach a leader in the hernia field the Shouldice technique. It is through visits like these and potentially through more innovative ideas, that we could perhaps have an impact on more surgeons throughout the country.
It is becoming more apparent that inguinal hernia anatomy teaching is lacking in the United States. It is my hypothesis that many of the poor outcomes after inguinal hernia surgery are less about the approach or the mesh that is used, and more about the surgeons’ technical knowledge and skill-set when repairing an inguinal hernia. After my time at the Shouldice Hospital, I have come to the conclusion that they have better outcomes than anyone else in the world due to the fact that they created a system where surgeons are thoroughly trained in hernia anatomy prior to performing surgery on patients. These visits have reinforced my suspicions that many of us in the United States lack this foundational knowledge when we finish our training and have had to learn it on our own. The visit by Dr. Rosen, as well as hiring Dr. Fullington, highlighted the fact that I am able to transfer my anatomical knowledge to other surgeons. Hopefully, as we collect more data from the ACHQC, we can prove that quality outcomes are reproducible when a deliberate process and curriculum is created for training surgeons.
The incidence of chronic pain after inguinal hernia surgery is a public health problem in the United States, but also an opportunity that can be addressed through systemic surgeon education. It is my belief that while not glamorous, teaching surgeons inguinal hernia anatomy is likely to produce better outcomes than teaching surgeons new techniques using newer and more expensive technology. It is my hope that over the next decade we will create a curriculum that is accessible to every trainee and surgeon in the United States to become better inguinal hernia surgeons, since it is the most common abdominal wall surgery performed in the US and around the globe.
——-
Drs Reinhorn and Rosen with Greg DeConciliis PA-C of BOSS (right)
Boston Outpatient Surgical Suites is an ambulatory surgery center in Waltham, Massachusetts. Founded in 2013 by Dr. Brian McKeon, who was the Boston Celtics team physician for over a decade. The center is led by Greg DeConciliis PA-C who also sits on the Massachusetts Association of Ambulatory Surgery Centers. With a distinct focus on providing high-value care to its patients and a positive work environment to its staff, BOSS is one of the highest rated and most efficient ambulatory surgery centers in New England.
Drs Reinhorn and Rosen joined by Greg DeConciliis PA-C
Boston Hernia is the private practice co-founded by Lauren Ott, PA-C and Dr. Michael Reinhorn, with offices in Wellesley, Massachusetts and Derry, New Hampshire. Boston Hernia provides care for patients throughout New England who are able to drive to one of the locations. Dr. Nora Fullington and Anna Canavan, PA-C joined the practice early in 2021 to expand the availability of the subspecialized care provided by the practice.
