Author: Kortney Hodgson PA-C
Boston Hernia Publishes Outcomes of Fast-Recovery Inguinal Hernia Surgery: Significant Improvement in Recovery Over Traditional Approaches
On August 8th, 2023, Boston Hernia was featured in a paper showing improved patient-reported outcomes after open preperitoneal inguinal hernia repair when compared to anterior Lichtenstein repair.
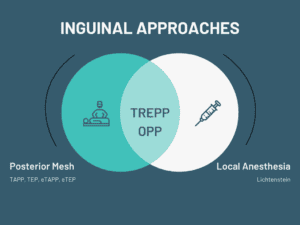
For four decades, the Lichtenstein repair has been the go-to option for “open” inguinal hernia repairs. However, international guidelines propose a shift towards posterior mesh placement, citing its biomechanical benefits and potential to mitigate nerve-related chronic pain. Furthermore, the use of local anesthetics can significantly diminish postoperative discomfort and minimize risks. Emerging as a potential game-changer, the open transrectus preperitoneal/open preperitoneal (TREPP/OPP) repair seamlessly combines posterior mesh placement with the utilization of local anesthetics, positioning it as the optimal approach to primary inguinal hernia repair.
Using the Abdominal Core Health Quality Collaborative (ACHQC) registry, we compared open anterior mesh with open posterior mesh repairs. Our analysis demonstrates the benefit of posterior mesh placement (TREPP/OPP) over anterior mesh placement (Lichtenstein) in open inguinal hernia repair in patient-reported quality of life and reduced opioid use.
At Boston Hernia, we specialize in the OPP/TREPP inguinal hernia repair, which is a posterior mesh repair that allows for fast recovery. This fast recovery repair is done through a small incision in the groin and is typically performed under local anesthesia with sedation when appropriate. This repair technique has been found to be an excellent alternative to laparoscopic or robotic surgeries, particularly for patients with a BMI under 33.
The application of this surgical approach holds the potential to revolutionize postoperative recovery for the majority of inguinal hernia patients, virtually eradicating the burden of chronic pain. At Boston Hernia, we hold a firm conviction that surgeons must pivot their attention from passively acknowledging chronic pain to actively striving to eliminate it as an accepted outcome. We hope for a transformation within the surgical community’s mindset. It is our belief that practitioners should engage in the education and training required for all forms of posterior mesh placement, rather than limiting themselves to options reliant on costly technologies, including laparoscopic and robotic procedures.
In publishing our paper within the medical community, we do so with a profound sense of purpose. Our intention is to guide and facilitate the adoption of posterior mesh placement techniques, transition to tailored surgical approaches sensitive to the needs of individual patients, and thereby usher in a new era of inguinal hernia surgery. By embracing these insights, we aspire to significantly decrease the risk of chronic pain following these procedures, enhancing the quality of life for patients receiving hernia care.
In conclusion, open approaches to posterior mesh placement in inguinal hernia surgery have improved outcomes over open anterior techniques. The combination of a minimally invasive open approach and optimal mesh placement has allowed for a new level of quality in inguinal hernia surgery, reshaping the trajectory of recovery for countless patients.
We appreciate the help from our colleagues at Massachusetts General Hospital in helping us perform this important research.
